Bedwetting Fact Sheet – Causes, Treatments, and Support for Families
Bedwetting (the medical term is nocturnal enuresis) is a common childhood issue that can affect young children, school-aged kids, and even some teenagers. As parents and caregivers, it’s normal to feel concerned or frustrated, but it’s important to know that bedwetting is usually not anyone’s fault and most children outgrow it with timehealthychildren.orgnewsnetwork.mayoclinic.org. This comprehensive fact sheet by Chooniez – a brand dedicated to helping families manage bedwetting and incontinence – will cover everything you need to know in a friendly, reassuring, and professional tone. We’ll explore all the possible causes of bedwetting (medical, psychological, genetic, and lifestyle factors), discuss treatment options from behavioral strategies to medical interventions, look at the emotional impact on children and families, and debunk some common myths. Throughout this guide, keep in mind that you and your child are not alone – millions of families face this challenge, and with understanding and the right approach, it can be managed and overcome.
What is Bedwetting (Nocturnal Enuresis)?
Bedwetting refers to involuntary urination during sleep in a person old enough to have bladder control. Doctors typically use the term nocturnal enuresis for bedwetting. It’s generally not considered a medical concern until around age 5 or 6, since bladder control at night is the last stage of potty training for many children archildrens.org. There are two main types of nocturnal enuresis:
- When a child has never been completely dry at night for at least 6 months in a rowmy.clevelandclinic.org. In primary enuresis, nighttime dryness just hasn’t been achieved yet – often due to developmental factors.
- when a child starts wetting the bed again after a long period of staying dry (at least six months or more)my.clevelandclinic.orghealthychildren.org. Secondary enuresis is less common and can be a sign of an underlying issue (for example, stress or a medical condition) that needs attentionhealthychildren.org.
It’s important to remember that bedwetting is involuntary. A bedwetting child is not being lazy or defiant – they simply cannot feel or respond to the urge to urinate while asleep. The brain-bladder communication during sleep is still maturing in children. In fact, doctors define nocturnal enuresis in diagnostic terms as nighttime wetting in kids 5 years or older at least twice a weekaafp.org. This definition helps distinguish a medical issue from the normal occasional “accident.” Many kids under 5 will wet the bed as their bodies and nervous systems develop, and that in itself is normal.
Monosymptomatic enuresis means bedwetting is the only symptom (no daytime accidents or other urinary symptoms), whereas non-monosymptomatic enuresis means there are daytime symptoms too (like urgency, frequency, or daytime accidents)aafp.org. This distinction matters because bedwetting with daytime urinary issues might indicate a different kind of problem (such as bladder dysfunction or other medical conditions) and would be handled differently by doctorsaafp.org.
Key point: Bedwetting beyond the typical potty-training age can be stressful, but it’s very common and usually not a serious problem. Understanding the causes and solutions will help you support your child. First, let’s see just how common bedwetting is for various ages.
How Common is Bedwetting?
If your child wets the bed, you might wonder, “Are we the only ones dealing with this?” Absolutely not! Bedwetting is a common developmental phase, and many families are going through the same thing. Here are some quick facts and statistics on how widespread bedwetting is:
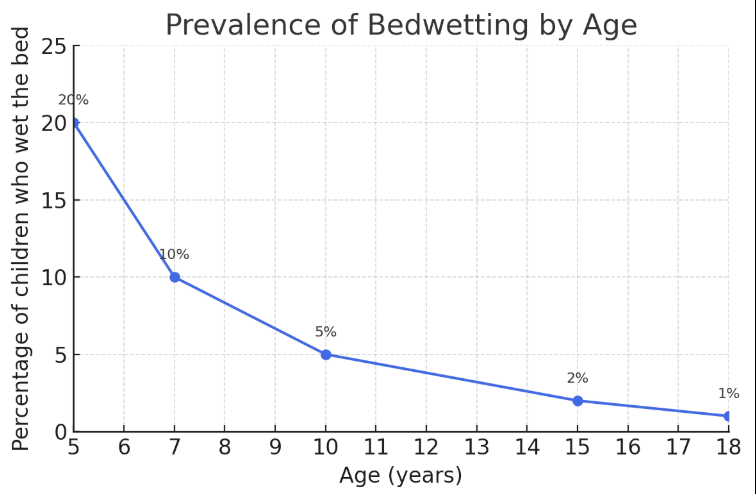
Roughly 15–20% of children at age 5 still wet the bed at least occasionallyhealthychildren.orgaafp.org. That’s about one in five kids – so in a class of 20 kindergarteners, a few are likely still bedwetting. Pediatricians consider bedwetting normal up to this age.
By about age 7, the percentage of kids who wet the bed drops to roughly 10%healthychildren.org. In other words, about one in ten 7-year-olds is not yet consistently dry at night.
Approximately 5% of 10-year-old children (1 in 20) still experience bedwettingarchildrens.org. So while most kids have outgrown it by this age, it’s not extremely unusual even in late elementary years.
It’s estimated that 1% to 3% of children in their late teens continue to have occasional bedwettinghealthychildren.org. Other sources put the figure around 1–2% by age 15archildrens.org. Bedwetting is less common in adolescence, but it does persist for a small minority of teens.
Bedwetting is 2 to 3 times more common in boys than in girlshealthychildren.org. No one knows exactly why, but this is a consistent finding across studies. Both boys and girls can be affected, but if you have a son who wets the bed, know that it’s even more common in boys.
The vast majority of people outgrow bedwetting by adulthood. Only around 0.5% to 1% of adults have persistent bedwettingaafp.org, though some studies report up to 2–3% of adults may occasionally experience itmy.clevelandclinic.org. It’s quite rare by this stage, often associated with specific medical issues if it continues.
Prevalence of bedwetting tends to decrease as children grow older. Around 20% of 5-year-olds wet the bed, but this rate drops to ~5% by age 10 and about 1–2% by age 15archildrens.org. The chart above illustrates how bedwetting becomes less common with age. Most children eventually outgrow bedwetting during adolescence, with only a small percentage affected in the teen years and beyond.
These numbers show that if your child is still bedwetting, they are truly not alone. In the U.S. it’s estimated about 5 to 7 million children age 6 or older wet the bed at least some of the timekidney.org. Every year, a portion of children stop bedwetting on their own – roughly 14% of bedwetting children achieve dryness each year without treatment just by growing and maturingaafp.org. So time is on your side in many cases, though it can require patience.
One more thing to consider is family history. Bedwetting has a strong genetic component. If you or the child’s other parent wet the bed as a child, there’s a higher chance your child will experience it too. In fact, studies show that if one parent wet the bed, the child has about a 40% chance of bedwetting; if both parents did, that chance rises to over 65–70%healthychildren.orgaafp.org. (By contrast, if neither parent wet the bed, the risk is much lower, around 15%aafp.org.) Enuresis also tends to resolve at similar ages within families, meaning a child might stop around the same age that their parent didaafp.org. So, if bedwetting “runs in the family,” it’s not because of poor potty training – it’s often due to inherited factors. This also means your child may outgrow it around the same age you or your relatives did.
The main takeaway: Bedwetting is common and often inherited, and most kids will eventually outgrow it. Next, we’ll look into why bedwetting happens – understanding the causes can help you approach the problem more effectively.
Best Incontinence Products
12 Causes of Bedwetting: Why Does It Happen?
Bedwetting can be frustrating to deal with, but remember that your child isn’t doing it on purpose. There are several potential reasons why a child might wet the bed. Usually it’s not due to any one “bad” thing – rather, bedwetting tends to happen when a child’s body is still developing certain abilities or when specific factors are at play. Below, we cover all the known causes and contributing factors for bedwetting, including medical, genetic, psychological, and lifestyle aspects.
In many children, bedwetting is essentially a result of a developmental delay in the nighttime bladder control mechanism. Think of it this way: staying dry at night requires a coordinated effort between the brain, bladder, kidneys, and hormones. If any one part of this system is a bit behind in maturing, bedwetting can resulthealthychildren.orghealthychildren.org. Here are the main factors that can cause or contribute to bedwetting:
- Delayed Brain–Bladder Communication: Some kids’ brains are not yet responding to the bladder’s signals at night. Normally, as the bladder fills, it sends a message to the brain saying “wake up and go to the bathroom.” In children who wet the bed, often the brain doesn’t reliably wake up to that signal yethealthychildren.org. These children tend to sleep very deeply and simply do not wake when they need to urinatehealthychildren.org. This is sometimes called an arousal disorder – the child’s sleep is so deep that the body’s cue to wake up doesn’t get through. There is nothing “wrong” with the child’s willpower – it’s a matter of the sleep cycle and brain maturity.
- Small Nighttime Bladder Capacity: Some children have a smaller functional bladder capacity at nightmy.clevelandclinic.org. Even if their bladder volume is normal in general, their bladder might signal “full” at a lower volume of urine during the night. If a bladder can’t hold all the urine produced overnight, it will empty (resulting in wet sheets). Think of it as the bladder’s “tank” being too small overnight. A child with this issue might also need to pee more frequently in the daytime and may have a strong urge to “go” suddenly during the daymy.clevelandclinic.org.
- High Nighttime Urine Production: Some kids produce a lot of urine at night – sometimes because their bodies don’t yet make enough of a hormone that helps concentrate urine. Normally, our brains release antidiuretic hormone (ADH) (also called vasopressin) during sleep, which tells the kidneys to make less urine at night. If a child’s body isn’t making enough ADH at night, their kidneys might fill the bladder with more urine than usual while they sleepmy.clevelandclinic.org. This can easily overwhelm a child’s bladder capacity. The result is that even if the child’s bladder capacity and sleep arousal are typical for their age, the sheer volume of urine makes them wet the bed. (This is a physical/biological cause – nothing the child can control.)
- Genetics and Family History: As mentioned, genetics play a role. If bedwetting runs in the family, a child is more likely to experience ithealthychildren.org. Researchers have even identified certain genes associated with enuresis. The inheritance pattern isn’t 100% predictable, but the risk is significantly higher when parents or close relatives wet the bed. Genetics can influence things like bladder size, depth of sleep, urine production, and when the brain-bladder connection fully matureshealthychildren.orgaafp.org. In short, bedwetting often runs in families – it’s an inherited developmental timeline in many cases.
- Deep Sleep Patterns: Some children are extra-deep sleepers, especially as they hit preteen and teen years due to growth and hormoneshealthychildren.org. If your child sleeps like a rock and is hard to wake, this could contribute to bedwetting because they don’t wake to the bladder signals. Deep sleep by itself isn’t a bad thing – it’s part of normal development too – but it can mean the child’s body doesn’t rouse them in time. (This factor overlaps with the brain-bladder arousal issue above.)
- Urinary Tract Infections (UTIs): A urinary tract infection can irritate the bladder and make it harder for a child to control urination, possibly leading to sudden onset of bedwetting or daytime accidents. If a child who was dry at night starts wetting the bed again frequently, or has pain while urinating, a UTI could be the causemy.clevelandclinic.org. UTIs are usually accompanied by other symptoms (burning with pee, frequent urgent need to pee, maybe fever or belly pain). Treating the infection typically resolves the wetting in these cases.
- Constipation: Surprisingly, constipation is a very common hidden cause of bedwetting. If the bowels are full, the packed stool in the rectum can press on the bladder, reducing the bladder’s capacity or irritating bladder nerveshealthychildren.org. Many doctors will ask about a child’s bowel habits when evaluating bedwetting. Chronic constipation can lead to nighttime (and daytime) wetting, and treating the constipation often greatly improves the enuresishealthychildren.org. If your child has infrequent BMs or hard stools, relieving the constipation might be one of the first steps to dry nights.
- Anatomical or Neurological Issues: In rare cases, bedwetting can be a sign of an underlying anatomical or nerve issue. For example, problems with the spinal cord or nerves (such as spina bifida occulta or other spinal abnormalities present from birth) could affect bladder controlhealthychildren.org. These conditions often have other signs like leg weakness, abnormal gait, or numbness. Another example is a physical abnormality in the urinary tract (like a urethral obstruction or an abnormally formed bladder). However, these causes are uncommon. Doctors may look for these if there are red flags like neurological symptoms or if a child has significant daytime bladder dysfunction in addition to bedwettinghealthychildren.org.
- Psychological or Emotional Factors: Stress and psychological factors do not typically cause primary bedwetting, but they can be significant in secondary enuresis (when an older child who was dry starts wetting again)healthychildren.org. Major life changes or emotional stressors can trigger bedwetting in a child who had been dry. Examples include family changes (divorce, new baby, loss of a loved one), moving to a new home or school, or bullying and anxietyhealthychildren.org. In these cases, the stress affects the child’s sleep and hormone balance, potentially leading to bedwetting. Treating or managing the stress often helps resolve the bedwettinghealthychildren.org. It’s worth noting that ordinary childhood emotions (excitement, minor worries) are not likely to cause bedwetting – we’re talking about significant stress or trauma. Importantly, bedwetting itself can create stress for a child, which can sometimes make the problem worse in a cycle, so providing emotional support is crucial (more on that later).
- Excess Fluid Intake in Evenings: Lifestyle habits can contribute to bedwetting severity. If a child drinks a large volume of liquids in the evening, especially right before bed, that increases the chances of a wet night simply by volume of urine. Caffeine or sugary drinks in the evening are especially problematic – caffeine is a diuretic (makes kidneys produce more urine) and can also disrupt sleep, and sugary or carbonated drinks can irritate the bladderhealthychildren.org. That said, a child who is prone to bedwetting will still wet even with normal fluid intake; heavy evening drinking just makes it more likely. Managing liquids (not eliminating them – just timing them earlier) can help (we’ll discuss this in treatments).
- Inconsistent Sleep Schedule or Poor Sleep: Not getting enough sleep or having an irregular sleep schedule can actually make bedwetting worse. An overtired child may sleep more deeply and be harder to arouse. Irregular bedtimes might disrupt the body’s hormonal rhythms (like the timing of that ADH hormone release). Ensuring a healthy sleep routine can sometimes improve bedwetting indirectly.
- “Too Busy” Bathroom Habits: Some younger children, in their daytime potty habits, don’t fully empty their bladder (maybe they’re rushing because they want to get back to playing). They might also avoid using the school bathroom, etc. Over time, if the bladder isn’t emptied completely, it could become overactive or less responsive. This isn’t a well-established cause, but healthy daytime bathroom habits (going every few hours and fully emptying) are recommended as part of managing enuresishealthychildren.org.
Major Causes and Contributing Factors in Bedwetting
| Category | Description & Examples |
|---|---|
| Developmental | Delay in brain-bladder connection maturing. Often associated with deep sleep patterns. The child sleeps deeply and doesn’t wake in time. |
| Bladder Factors | Small functional bladder capacity or overactive bladder at night. May include frequent or urgent daytime urination. |
| Hormonal | Low nighttime ADH hormone (vasopressin). Body doesn’t reduce urine production at night, resulting in increased urine output. |
| Genetic | Family history significantly increases risk. Bedwetting often runs in families, indicating an inherited developmental timeline. |
| Medical Conditions | Urinary tract infections, chronic constipation, diabetes, anatomical abnormalities, neurological issues (e.g., spinal cord conditions), and rarely, sleep apnea. |
| Psychological | Stressful life events (e.g., moving, parental divorce, new sibling, bullying) can trigger bedwetting, especially secondary enuresis. |
| Lifestyle & Habits | Excessive evening fluids, especially caffeine or sugary drinks; irregular bedtime routines and poor sleep hygiene. |
| Attention/Neuro | Children with ADHD or developmental delays have higher incidence of bedwetting, possibly related to differences in sleep or neural development. |
The Emotional Impact on Children and Families

Bedwetting doesn’t only wet the sheets – it can also bring a wave of emotions for both the child and the family. Understanding the emotional impact is important, so you can help your child cope and ensure the issue doesn’t harm their self-esteem.
How children may feel: Many children feel embarrassed or ashamed about wetting the bedhealthychildren.org. They might worry that something is wrong with them. If they’re old enough to understand, they could feel like they’re the only one their age who still wets the bed (even though, as we saw, it’s fairly common). This embarrassment can make kids very self-conscious. For instance, children often start avoiding sleepovers, camping trips, or overnight activities because they fear their friends will find out and tease themhealthychildren.org. A child who really wants to go to a pajama party may decline the invitation, or go but then try desperately to hide any evidence of an accident. This can be socially isolating – they miss out on fun experiences due to the fear of an accident.
Bedwetting can also lead to anxiety in children. They might start feeling anxious every night at bedtime, worrying “will I wet the bed again?” This anxiety can ironically make sleep worse, which doesn’t help the situation. Some kids develop low self-esteem or feel like they are “babies” for still wetting the bedhealthychildren.org. If siblings or peers tease them (even innocently), it can really hurt. It’s not uncommon for a child to say things like, “Why can’t I be like other kids?” or “I’m too old to be in diapers at night”, feeling very down on themselves.
How parents may feel: For parents and caregivers, bedwetting can be stressful and tiring. Constantly washing sheets, waterproof mattress covers, and pajamas can become a significant extra chore. It can be frustrating when despite your best efforts (limiting drinks, waking the child at night, etc.), the bed is wet again in the morning. You might worry if you’re doing something wrong, or if your child is having this issue because of something you did or didn’t do (rest assured, in almost all cases, that’s not true). There can also be a sense of helplessness – you can’t “fix” this immediately for your child, and seeing them upset can hurt.
If the child shares a room, siblings might have to deal with disrupted sleep (for example, a loud alarm going off at night or a parent coming in to change sheets) or might feel annoyed or confused. It’s important for siblings to understand the situation so they don’t blame or tease the bedwetting child.
Behavior and family dynamics: Sometimes, frustration can lead family members to shame or scold the child out of desperation. It’s critical to avoid this. Punishing or shaming a child for bedwetting is not only ineffective – it can worsen the problemarchildrens.org. Remember, the child is not wetting the bed deliberately, so punishment only adds stress and lowers self-esteem, which can prolong bedwettingarchildrens.org. Children who feel ashamed or fear punishment may become secretive – for example, hiding wet pajamas or sheets – which adds even more anxiety.
On the other hand, a supportive family approach can make a huge positive difference. Children should be reassured that they are not “bad” or doing anything wrong by wetting the bedhealthychildren.org. Explain to them (in age-appropriate terms) that this is a common, fixable issue. For instance, you might say, “Your bladder is still growing and learning, and that’s okay. Lots of kids take time to stay dry at night.” Knowing that their parents are patient and understanding can relieve a lot of the child’s worry.
Parents might also feel embarrassed to discuss the issue outside the home. But talking to your pediatrician is very important – don’t hesitate to bring it up. Doctors discuss bedwetting all the time and can offer guidance and reassurance. There’s no need to keep it a secret or “live with it” in shame. Support groups or online communities (for example, forums for parents of kids with enuresis) can also help parents feel less alone and share tips and encouragement.
Quality of life: Studies have shown that children with enuresis can have lower self-esteem and quality of life compared to their dry peersaafp.org. The good news is that when bedwetting improves or is successfully treated, those quality of life measures (mood, self-confidence, etc.) improve as wellaafp.org. This is why addressing the issue – not ignoring it – is important for a child’s emotional well-being. Even if we choose to “wait it out” for the child to outgrow it, we should still support the child emotionally in the meantime.
Debunking 8 Common Myths about Bedwetting
Fact: Bedwetting is involuntary. It happens during sleep, when the child’s conscious control is absent. Children do not wet the bed on purpose or out of lazinesshealthychildren.org. In fact, most kids who wet the bed desperately wish they didn’t. The cause is usually physical/developmental (deep sleep, small bladder, etc.), not behavioral. Your child is not being “bad” – and you cannot train bedwetting out of them by scolding or discipline.
Fact: Punishment never helps bedwetting – it can actually prolong the problemarchildrens.org. The child already feels bad; adding shame increases stress and can worsen enuresis. Similarly, making fun of or embarrassing a child for wetting will likely decrease their self-esteem and trust, without solving anything. Positive encouragement and patience work far better. Bedwetting is a medical/developmental issue, not a discipline issue.
Fact: Bedwetting is very common in young kids, but it’s not unusual for older kids and even teens to have this issue. By age 7, about 10% of kids still wet the bed, and by the late teen years, up to 3% may still occasionally wet the bedhealthychildren.org. While it’s true that most children outgrow bedwetting by adolescence, a school-age child or teenager with enuresis is not “freakish” – they are within a known percentage of kids who simply take longer to develop nighttime control. Often, there’s a family history or a treatable cause. The important thing is to approach it as a solvable problem, not to panic or make the child feel abnormal.
Fact: During sleep, the usual conscious control is off. Many bedwetting children are deep sleepers who truly do not sense the bladder signals. This is a physiological thing – not about willpower. In fact, some kids even dream that they’re on the toilet because the brain is partially signaling them, but not enough to wake up fully. You can’t train the brain-bladder connection overnight by willpower. However, tools like bedwetting alarms can gradually train the child’s body to recognize the need to wake up (more on this in Treatment section)healthychildren.org. But without such interventions, a child can’t simply will themselves to wake – if they could, they would have already done so!
Fact: It’s not necessary to totally forbid fluids after a certain time. Children should have a reasonable amount to drink with dinner and if thirsty later – hydration is important for health. The sensible approach is to moderate evening fluids, especially avoiding drinks 1–2 hours before bedarchildrens.org, and to skip known bladder irritants (caffeine, sugary sodas) late in the dayhealthychildren.org. But making a child go to bed thirsty or dehydrated is not healthy or kind. A small sip of water if they’re very thirsty at night is okay. Focus more on establishing a habit of using the toilet before bed. Extreme fluid restriction is usually unnecessary; moderation is key.
Fact: Bedwetting is nobody’s fault – not the child’s and not the parents’. It’s often a matter of maturation or genetics, which parents cannot control. Toilet training success during the day also does not guarantee dry nights, because nighttime continence is a different developmental milestone. You could do everything “perfectly” in terms of potty training and still have a bedwetter. Conversely, a child with less ideal potty training could be dry at night if their body is ready. So do not blame yourself or your parenting for your child’s bedwetting.
Fact: Most children do outgrow bedwetting with timenewsnetwork.mayoclinic.orgnewsnetwork.mayoclinic.org, but that doesn’t mean you have to simply suffer through it until then. If bedwetting is causing distress to your child or family, or if the child is already 6-7 or older and wants to be dry, there are many effective strategies and treatments that can help speed up the process or manage the situation in the meantime. It’s perfectly reasonable to seek help. Moreover, if bedwetting starts suddenly after a period of dryness or is accompanied by other symptoms, you definitely should consult a doctor (because it could be a sign of an underlying issue). So while patience is important, active management can vastly improve quality of life.
Fact:Medications for bedwetting (we’ll discuss them soon) can be very helpful in certain situations, but they typically do not “cure” bedwetting permanently – when the medication is stopped, the bedwetting often returnshealthychildren.orgnewsnetwork.mayoclinic.org. The only real “cure” is time or behavioral conditioning (like alarms) that trains the body. Alarms have the best long-term success rates for permanently resolving the issueaafp.orgaafp.org, whereas medications are usually a temporary management tool (useful for events like sleepovers or camps, or for older kids as a bridge to outgrowing the problem). Each child may respond differently, and sometimes a combination is used, but it’s not true that pills are a magic bullet cure – nor that alarms “don’t work” (they do, with persistence).